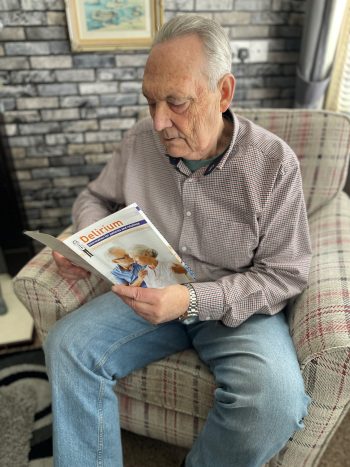
“I found I was not eating, I wasn’t sleeping. Everything just seemed to change for me.” These are the words of 76-year-old Bill Cheevers who has thanked staff at the Ulster Hospital following a Delirium diagnosis in January 2025.
After being discharged from hospital following a UTI infection, Bill was readmitted following a fall at his Millisle home. Bill was unaware that he was experiencing signs and symptoms of Delirium through lack of sleep, appetite and becoming withdrawn from family.
Bill explained that when doctors told him he had Delirium, he is now better equipped to look out for signs associated with illness,
“I was quite taken aback when I was told I had Delirium. I am now involved in a working group in the Ulster Hospital with the Ward Sisters and I have a plan in place with my GP, I now feel more informed about Delirium,” said Bill.
South Eastern Trust Consultant Psychiatrist Dr Pratibha Nirodi detailed how the majority of patients in an acute hospital setting, especially the elderly, have confusion. Dr Nirodi explained how the main signs of Delirium are, “Confusion, agitation, drowsiness and hallucinations.”
“One in three older adults in hospital experience Delirium,” said Dr Nirodi. “
“The first thing relatives and staff can do is look for signs to see if that person is more confused than they normally are.” “The risk is increased for those aged 65 and over, through infection, fractures, surgery, long hospital stays or medication changes.”
“If we can prevent people from becoming delirious, then that can reduce their hospital stay or potentially that person going into a care facility. If we can recognise delirium, whether it’s at home or whether it’s in a care facility early – we can treat it early.”
Dr Nirodi stressed that a checklist is in place called ‘PINCH ME’ to prevent a patient experiencing delirium.
“P is to firstly recognise if that person is in pain, I is to look for any signs of an infection, N is for nutrition – is that person eating their meals? C is for constipation, H is for hydration, M is for medication and E is for environment. It is much better to have a room, an environment with familiar objects if that person has been brought into hospital, a simple thing like a large clock helps tremendously in keeping with the time, day and date.”
Dr Nirodi added how specific treatment methods can help for those experiencing delirium. “We can all play our part, especially family members in keeping the patient calm when they are in hospital, through ensuring patients eat and drink and making the setting as familiar as possible.”
When asked what his advice would be to anyone who may be experiencing signs of Delirium, Bill added, “Seek medical help, you just know yourself when you are not right and you feel within yourself that you are not right. Go to your GP or attend hospital to get checked out.”
Six months on from his diagnosis Bill is now on the mend. “You just carry on. Life returns to normal.”





